The Test of Time: Acute versus Chronic Aortic Dissections
Time brings all things to pass.
— Aeschylus
Introduction
Aeschylus (c. 525/524 – c. 456/455 BC) was an ancient greek tragedian who was called the “father of tragedy”.
Perhaps, Dr. Michael DeBakey, the world-renown heart surgeon from Methodist Hospital in Houston, could be considered the modern father of aortic dissection.
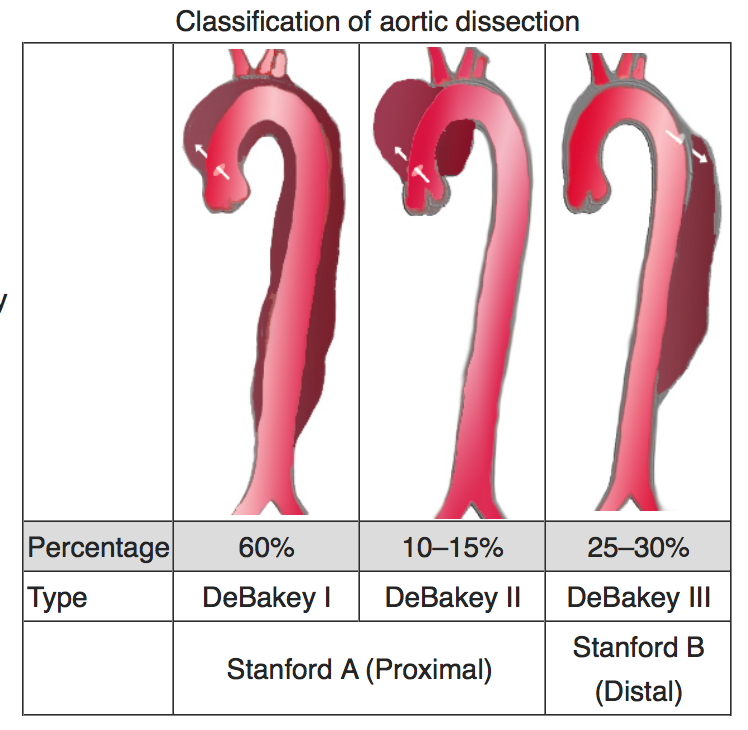
Dr. DeBakey’s classification of aortic dissections is still used today to describe the different ways that aortic dissections manifest.
In the spirit of Aeschylus, and with a nod to Dr. DeBakey, let’s discuss ACUTE versus CHRONIC aortic dissections.
Definitions
You may want to refresh yourself about aortic dissection from our previous posts HERE and HERE. Aortic dissection is a complex disease with many different forms of presentation. It is a spontaneous process which develops literally within a few heart beats. Because aortic dissection seems to come “out of the blue”, many patients are baffled about how they developed this problem.
Let’s be real. Patients can be walking around, with everything normal, and suddenly collapse with an instantaneous episode of disabling chest or back pain. Like many people with heart attacks, the sudden tearing of the layers of the aorta frequently develops without warning.
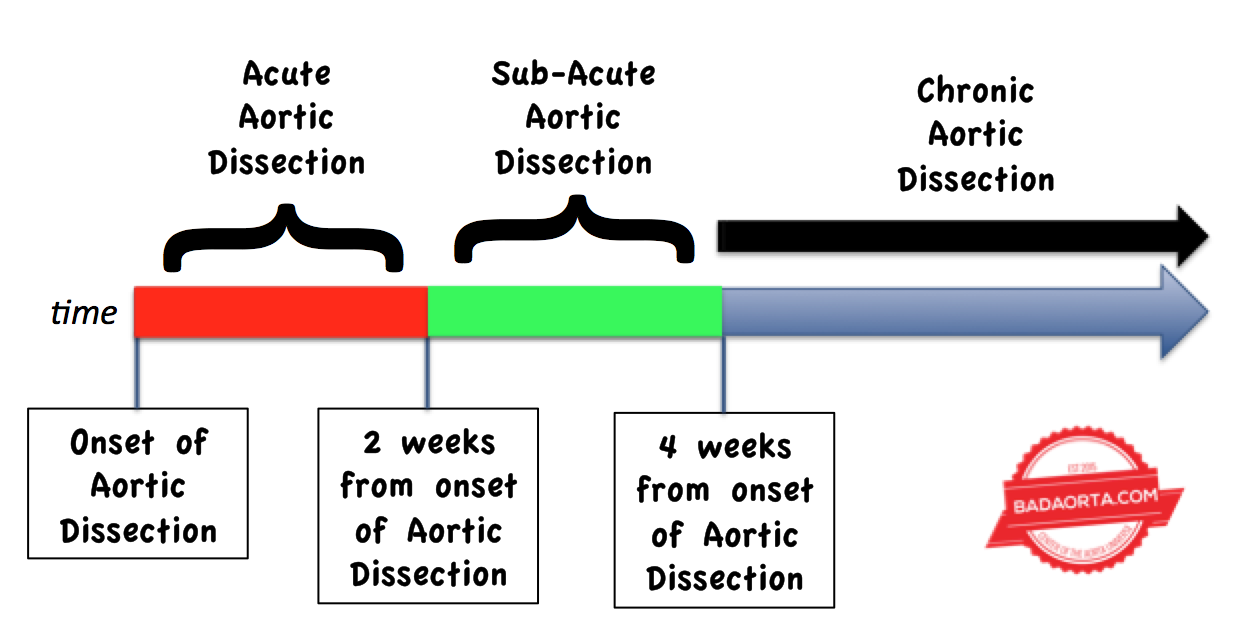
An ACUTE aortic dissection means that the dissection has been diagnosed within 2 weeks of the aortic dissection occurring. In fact, many patients are diagnosed in the emergency room within hours of the start of the aortic dissection.
Sadly, many patients with aortic dissection experience such a catastrophic series of emergent medical problems related to the aortic dissection, that they die instantly and never make it to the emergency room.
A CHRONIC aortic dissection refers to an interval of 4 weeks or more from the time when the aortic dissection started.
Later in this post, you will discover the medical and surgical implications of ACUTE versus CHRONIC aortic dissections.
Classification of aortic dissections
There are two major classification systems used to categorize the way aortic dissections occur. The underlying variables in both of these classification systems are:
-
In what part of the aorta (anatomically) does the aortic dissection start?
-
How much of an extent does the aortic dissection extend beyond the starting point?
As you recall from our previous post HERE, there are 4 main anatomic regions of the aorta: ascending aorta, aortic arch, descending thoracic aorta and abdominal aorta.
It is rare (but not impossible) for an aortic dissection to begin in the abdominal aorta. The entry tear (location where the ripping of the aortic layers begins) usually develops in either the ascending aorta or descending aorta. Aortic dissections can start in the aortic arch, but much less frequently.
The DeBakey and Stanford Aortic Classification systems are pictured below.
As you can see, there are a number of similarities between the classification systems.
ACUTE aortic dissections
Once again, an ACUTE aortic dissection refers to a 2 week interval from the time of onset of the aortic dissection. This 2 week interval is a very critical period in many ways. Within the first 2 weeks, the newly torn aorta is extremely fragile and prone to rapid deterioration. The initial line of treatment for acute aortic dissections is to control the blood pressure with medications.
Keeping the systolic blood pressure in a “normal” range (110-120 mmHg) lessens the chances that the tearing of the aorta could continue. Patients are almost always started on intravenous blood pressure medications (B-blockers) to immediately decrease the strain on the aorta. It is the physiologic pumping of blood within the aorta by the heart that continues to rip the aorta.
Even with optimal medical therapy (blood pressure control), the aortic dissection can worsen. Patients with acute aortic dissections are monitored in the intensive care unit, and have frequent examinations by nurses and physicians.
Patients with acute Stanford Type A aortic dissections are rushed off from the emergency room directly to the operating room for emergency open heart surgery.
Patients with acute Stanford Type B aortic dissections are evaluated for potential complications associated with the aortic dissection. Complications, such as sudden loss of blood flow to an important branch vessel off the aorta due to the dissection flap blocking blood flow to the vessel, require immediate surgical or interventional treatment in addition to medical therapy.
Other potential complications associated with an acute type B aortic dissection are resistance to the blood pressure medications or blood leaking from the torn aorta (hemorrhage). Once again, these complications require urgent treatment.
In a majority of circumstances, an acute type B aortic dissection will respond to medical therapy with blood pressure medications and not involve surgery.
CHRONIC Aortic Dissections

When an aortic dissection has been present for more than 4 weeks, then we call this a chronic aortic dissection. Remember, almost all Type A aortic dissections undergo emergency open heart surgery, so when we are discussing CHRONIC Type B aortic dissections, we are referring to patients with residual aortic dissections after their open heart surgery or Type B aortic dissections.
The significance in a dissection becoming CHRONIC, is that the whole torn aorta stabilizes and the body stabilizes the condition. This means that the torn tissues become more rigid and less likely to tear again or continue tearing (although that can rarely happen).
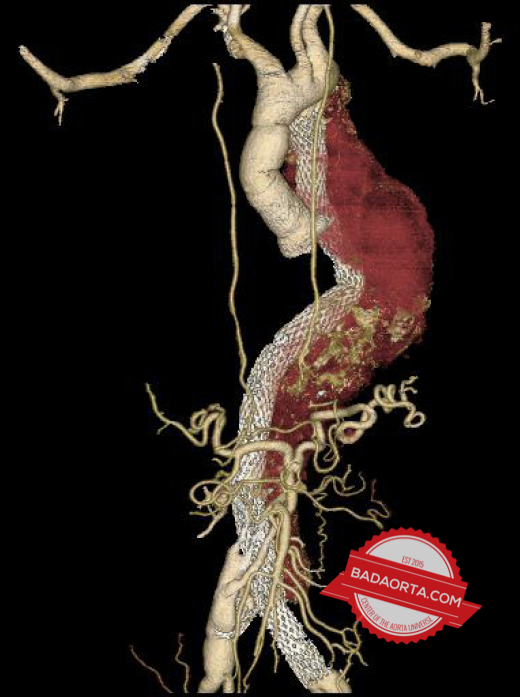
Approximately 1/3 of patients with chronic aortic dissections will experience slow expansion of the torn aorta. This expansion refers to a localized bulge of the aorta because of the weakened tissues. These patients can develop an aneurysm of the false lumen (blood channel created by the aortic dissection).
As a result, patients with chronic aortic dissections should be followed for life with annual CAT scans to detect this potential problem.
Implications for treatment
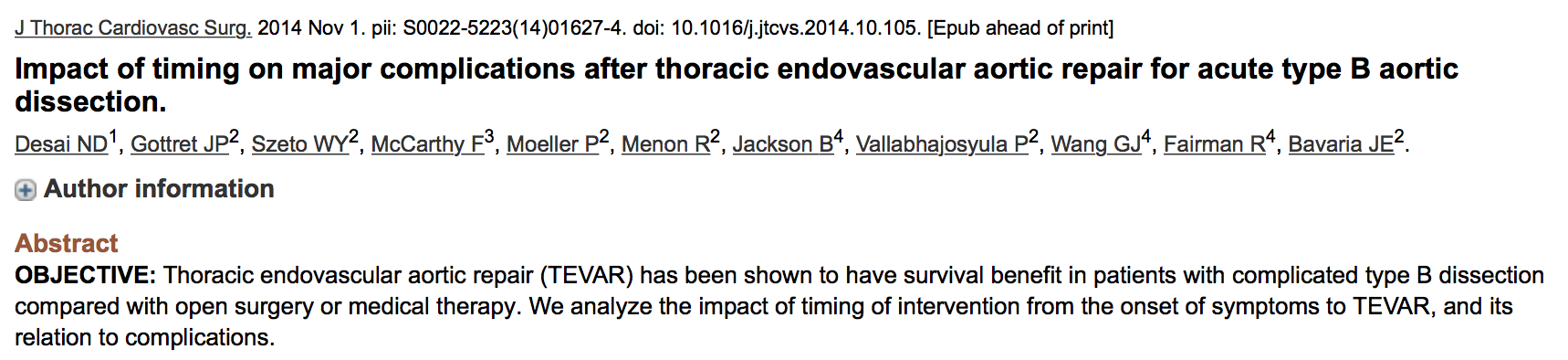
There is some early data to suggest that treating patients with aortic dissections in the “subacute” (2-4 week window) may be optimal.
Some authors are concerned that treating chronic aortic dissections with aortic stents may have limited efficacy, although others, like myself, believe that chronic aortic dissections can be treated successfully with an aortic stent-graft.
Summary
Aortic dissections are classified according to a number of variables including location of the tear, length of aorta affected by the tear and the duration of time since the tear originated.
All of these variables have an impact on the way that a particular case of aortic dissection is treated.
Question
Do you know anyone with an aortic dissection? Have you personally experienced and aortic dissection?
Comment and share your story so that other people can learn from your personal experiences.
PS. Don’t miss out. Download your FREE copy of Risk Factors for Developing Aortic Disease.
Was this post informative?
Subscribe to my newsletter to learn more about the aorta, its diseases, and how to treat them.
Comments
Share your thoughts below — I try to get back to as many comments as possible.