An Open Letter to Patients with Aortic Disease
I want to share with you - patients who have been diagnosed with an aortic problem - information about your disease that I tell all of my patients.
It is important that, in addition to understanding the complex anatomy and subtle decision-making process regarding the treatment of aortic diseases, that you also understand the implications of what you are being told.
Shock and awe
Being diagnosed with an aortic problem usually comes as a surprise. Most patients are completely unsuspecting that there is a potentially life-threatening problem lurking deep in their chest or abdomen.
It takes time for patients and their family members to reconcile what they have just been told. Many patients react with shock and disbelief. The frequent lack of symptoms associated with aneurysm disease makes it difficult to comprehend the magnitude of what lies ahead.
If you think about it, most patients go to the doctor when they feel ill and go through testing to identify the problem.
However, with aortic disease, the aortic problem, such as an aneurysm, usually shows-up as an “incidental” finding when testing is ordered looking for another problem.
Incidentally speaking
Unfortunately, “incidental” is a poor descriptor. An aortic problem is anything but an “incidental” medical condition.
When telling a patient that they have just been found to have an aortic problem, I am prepared for denial and minimization, which are natural reactions. I usually repeat myself a couple of times to make sure the information truly registers.
Immediate decisions are sometimes needed
If I am seeing a patient in the emergency room and they are just learning about their diagnosis, there is usually a need to make some quick decisions.
If the aneurysm is leaking, for example, or the aortic dissection starts in the ascending aorta (Type A), then immediate surgery is needed. There isn’t much time to understand anything more than what the surgery is and what the risks are (sometimes major risks).
In the clinic, immediate action is usually not required. In this setting, there is time to discuss and review all of the information.
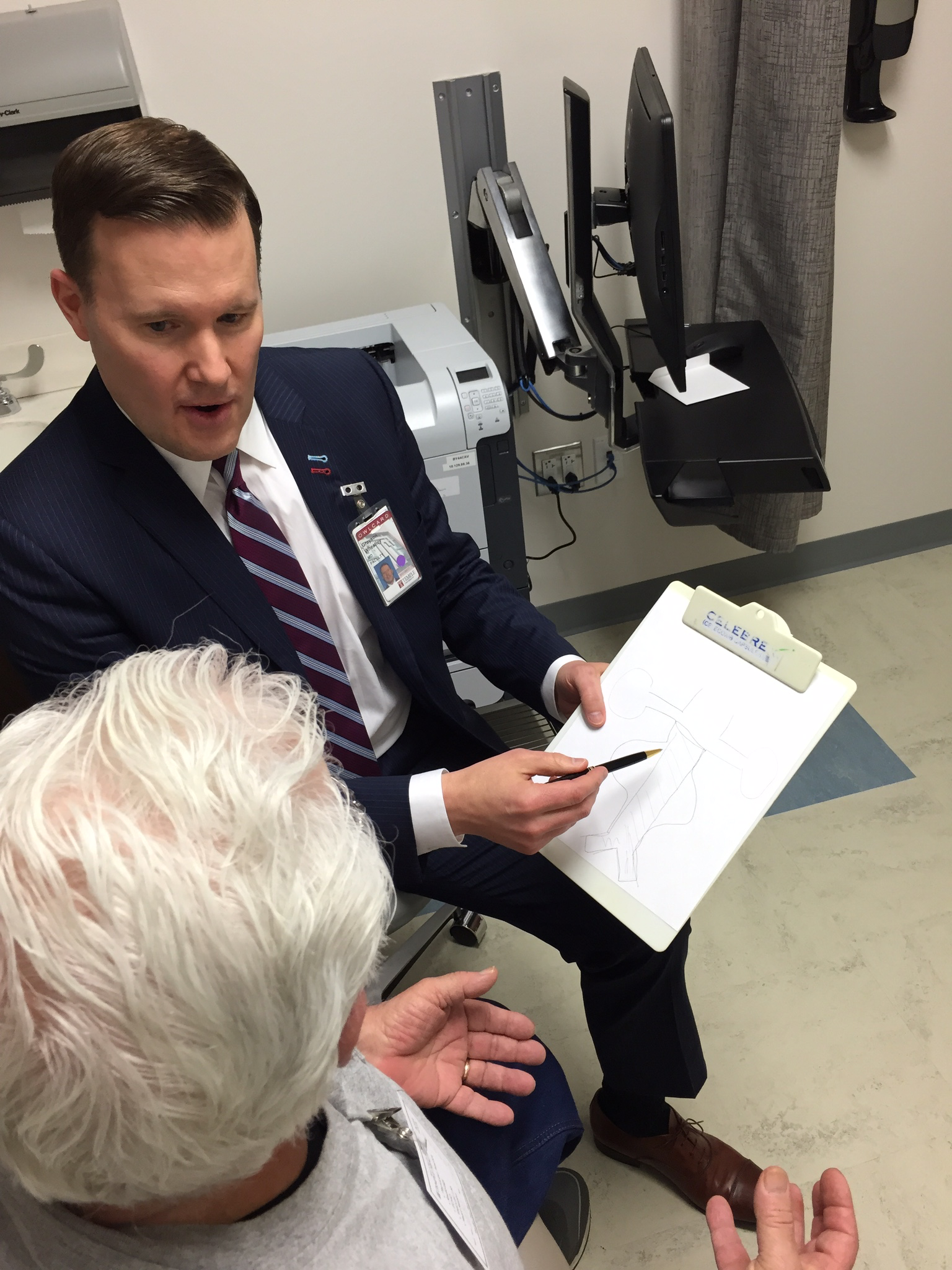
Clinic
I begin by explaining that the aorta - the largest blood vessel of the body - begins in the center of the chest at the connection to the heart (aortic valve, specifically) and initially heads upward toward the head before curving around behind the collar bones (clavicles) and descending deep in the chest back by the spinal column.
Next, I relate that the aorta anatomically extends into the stomach region (abdomen) and splits into two smaller branches at the level of the belly button (umbilicus). These two branches represent the beginning of blood supply to the lower extremities.
The aorta is usually an inch to an inch and a half in diameter. The natural size of the aorta is determined by several factors including height, weight and family history. There are probably other factors, but scientists are still investigating all the genetic components which lead to aortic disease.
I then spend time explaining their specific aortic problem. If the patient has an aneurysm, I discuss whether it is in the chest or abdomen and explain that the risk to them is the risk of sudden rupture of the aneurysm. I explain that sudden rupture means internal bleeding and almost certain death.
I discuss that the risk of a particular aneurysm is determined by the maximal width (diameter). A cutoff of 2 inches (5cm) in maximal diameter (width) is, in general, a threshold which requires a deeper dialogue about time to treat the problem. [Different regions of the aorta have different size cutoffs for treatment, but in general the 5cm applies to most regions of the aorta.]
The 5cm cutoff is not some arbitrary number, but is derived by numerous research studies. The 5cm cutoff is not always an absolute threshold, but must be factored into a broader consideration of the patient’s health and associated medical problems.
Aortic disease is a chronic medical problem
Regardless, I communicate that the diagnosis of an aortic problem represents a new, chronic medical condition for them. Like diabetes, they will need lifelong follow-up and monitoring. Even if the problem is successfully treated, they will need annual checkups and CAT scans.
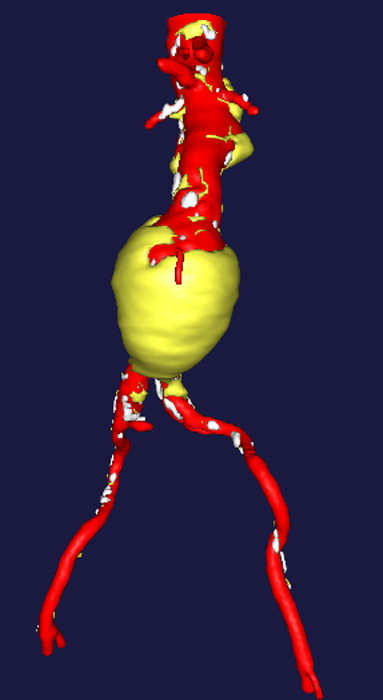
There are several reasons for this. First, whether the treatment for the aortic problem is surgery or endovascular stenting (EVAR or TEVAR), there are rare instances where those treatments breakdown overtime. This breakdown frequently is not associated with any symptoms and the only method of identifying these problems are with CAT scans.
Second, with regards to endovascular aortic stent-graft repair, the aneurysm is “excluded” by the aortic stent. This means that the aortic problem is left in place, but an aortic stent sits inside the aorta and becomes the “new aorta”. If the stent slips, moves or shifts overtime, then the aneurysm could become a problem. The only way to detect this is with annual check-ups.
Third, aortic disease is a systemic disease. Once an aortic problem is diagnosed, there is a significant chance that another aortic problem could arise later in life. Aortic disease is associated with aging. Therefore, many of the existing medical reasons that created an aortic problem will potentially create a second aortic problem.
Fourth, patients with aortic disease are at risk of developing not just aortic disease, but other cardiovascular diseases such as heart disease, carotid disease or peripheral vascular disease in the leg arteries. An aortic check-up will also screen for these other associated diseases.
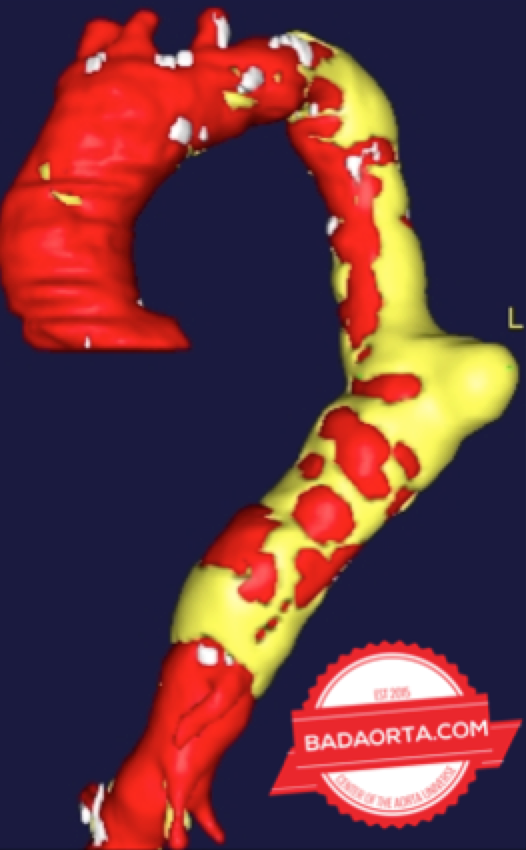
Fifth, particularly in patients with an aortic dissection, the aortic problem is never completely “fixed”. An aortic dissection involves a tearing apart of the layers of the aorta. Many patients can live a normal life with the torn aorta. If the torn aorta is fixed, it usually is only the part of the aorta where the tear starts. The remainder of the torn aorta stays in its torn state. Therefore, the surgically repaired aorta and the torn aorta both need surveillance with annual check-ups.
Sixth, most aortic disease is not initially treated. It is managed, not necessarily treated. Aortic disease is most frequently picked-up as an incidental finding on radiographic tests which are ordered looking for another potential problem. Many of the aortic problems which are identified are identified early in the course of development. In these cases, it is common to watch the aortic problem and proceed with annual check-ups.
Lifelong surveillance
When an aortic problem is found at an early stage (for example, size less than 5cm in diameter for an aneurysm) it is important to control the blood pressure. Even in patients who have not been diagnosed with hypertension, starting a low-dose anti-hypertensive medication to keep the systolic blood pressure less than 130mmHg can help slow or prevent progression of the aortic problem.
Next, if the aortic disease requires treatment, I discuss the potential treatment options. Frequently, there are two options: open surgery or endovascular repair.
However, if the aortic problem is in the aortic root, ascending aorta or even the aortic arch, surgery is the preferred and only method of treatment. For high-risk patients who have no surgical options, endovascular treatments can sometimes be offered.
For the descending thoracic aorta and the abdominal aorta, endovacular aortic stents are usually the best option.
However, this is an individualized decision and the final choice must result from an in-depth discussion between the patient and their aortic-expert.
I then pause and listen. By this time, patients and their families have numerous questions and I take the time to answer each question.
Finally, I summarize everything briefly and reiterate that we will need to go over all this information again. It is a lot to digest in one sitting.
In conclusion
Being diagnosed with an aortic problem is challenging from many perspectives. It takes time (and repetition) to understand the implications of the disease - from anatomy, to treatment, to lifelong surveillance.
It is my hope that this open letter to patients with aortic disease helps in someway toward a better understanding.
Was this post informative?
Subscribe to my newsletter to learn more about the aorta, its diseases, and how to treat them.
Comments
Share your thoughts below — I try to get back to as many comments as possible.