A Day in the Life of an (Innovative) Aortic Surgeon (Part One)
What does an Aortic Surgeon really do?
What is a typical day like for an Aortic Surgeon?
I get these questions a lot from patients and readers of BadAorta. Understandably, from a patient’s perspective, it is somewhat mysterious what we do and how we do it.
Consistent with the spirit and mission of BadAorta - to pull the veil back on all things Aorta - I wanted to share with you what a typical day at work is like for me.
Getting Started
I typically arrive to the hospital around 6:45am.
I roll into the parking garage and am greeted every morning by Joe, our smiling security guard. Rain or shine, Joe is standing watch on all the physicians, staff and patients who arrive to the hospital. He always has a smile and wave - never fail. It is a great way to start my day by saying good morning to Joe.
The parking garage is right across the street from the hospital. There isn’t a connecting walkway or tunnel, so if it is raining or snowing, I hustle across the side street separating the parking garage from the hospital entrance in order not to get too wet. I am not a fan of umbrellas.
I head into the hospital and walk right past the coffee shop. At this time of morning, there is usually a steady stream of hospital employees standing in line at the coffee shop awaiting their caffeine of choice.
I greet another security guard inside the front entrance. I take the stairs up one floor to the Pre-op Holding Area. This is the area where all the patients having surgery in the morning are prepared for surgery.
Teamwork
I greet my patient and each of the patient’s family members in the Pre-Op Holding Area waiting for surgery with a smile and a handshake. I am very focused on the upcoming surgery, but I know that meeting their surgeon immediately before going into surgery is an important moment that patients and family members will remember.
I am respectful of the trust that they have put on me so I lighten-up my focus on the upcoming surgery for a moment when I greet the patient to make sure I communicate effectively and address all their needs.
A time for tears
This is usually a time of anxiety and sometimes there are tears by the patient or their family members. I do my best to reassure patients.
When I arrive to the patient’s bedside, there are several people waiting for me. The patient and their family members are there. The nurse getting my patient ready for the OR, my anesthesiologist, an anesthesiology resident, my surgical first assistant and a medical student are also standing at the patient’s bedside. It is important that I efficiently and clearly speak with everyone individually about their role in the upcoming case and my communicate my expectations for them.
This process is not unlike a basketball coach during a timeout with his team huddled around him and he is drawing up plays to win the game with his players and assistant coaches listening intently.
The Operating Room start time is 730am for first cases. That means the patients leave the Pre-op Holding Area and are transported into the Operating Room at that time, not that the surgery actually starts right at 730am.
Patients and their families are contacted the night before surgery and informed what time they need to show-up at the hospital. Understandably, this is pretty early in the morning ( around 6am). I usually tell patients to look at the bright side, there is usually no traffic on the roads at that time and their trip into the hospital should be pretty smooth.
When a patient arrives to the hospital, they need to be registered, checked in and then directed to the Pre-Op holding area.
Blood bank

In the Pre-Op holding area, patients are disrobed, put on a hospital gown. There is a standard checklist of questions the nurses must go through and their medical records are updated if there have been any changes. IVs are also placed and blood specimens are drawn and sent to the blood lab.
For all aortic procedures, we need to have multiple units of blood available. The blood bank handles all those arrangements, but the patient’s blood has to be typed and cross-matched. The patient’s blood type is know beforehand, but there are multiple other components in the blood that need to be accounted for when choosing a compatible unit of blood.
Getting the blood ready can only be done on the morning of surgery and usually takes an hour. Therefore, we try and draw that blood sample as early as possible when the patient arrives in order to give the blood bank enough time to process the samples and locate the necessary units of blood.
The appropriate units of blood need to be physically located and held for that specific patient in the blood bank. Think about it, when a patient needs blood during surgery, it is usually needed quickly and we can’t allow a delay in trying to scramble to find a unit of blood during surgery. At the end of the procedure, if the blood units are not needed, then they are returned to the general pool to be used by another patient with similar blood type.
Sometimes there are delays associated with typing the patient’s blood and locating the appropriate units of blood. If this occurs, we delay going back to the operating room until we know the blood is available. It is that important!
Pre-op checklist
When I arrive to the pre-op area, all the items on the standard pre-op checklist have been completed by the nurses, all the paperwork has been completed, blood samples have been drawn and IVs have been placed. Hospitals have a very extensive patient safety process used to ensure that everything goes smoothly for the procedure.
In addition, the anesthesiologist and their team have also met the patient, had a conversation about the anesthesia and reviewed the medical record. Anesthesiologists with special training in heart and vascular surgery, called cardiac anesthesiologist, are used for aortic procedures.
The anesthesiologist has already set-up their station in the operating room. Like airline pilots, they check all the anesthesia machines ahead of time, check their inventory of medications and prepare special mixtures of medications in the room on the day of the surgery before the patient arrives into the operating room.
Consent
Consent for the procedure has already been obtained when I saw the patient in clinic. Nevertheless, when I greet the patient in the Pre-Op Holding Area the morning of surgery, I go over the procedure again briefly and discuss the risks again just to make sure the patient understands everything. As we have discussed before, there is so much information to process by the patient undergoing an aortic procedure (aortic anatomy, surgery procedure, recovery and follow-up), that it often takes several presentations by me for the entire process to sink-in.
Usually there are family members waiting at the bedside when I arrive to greet the patient on the morning of surgery. Many of these family members weren’t at the initial office consultation and haven’t met me or heard from me what the procedure involves. Therefore, it is very helpful for everyone that I go over the details of the procedure (again) so these new family members can understand what is going on.
After talking with the patient and their family, I tell them that everything is going to go well and give them two thumbs-up. I believe that it is important to provide patients and their family members with a strong, confident and supportive message before they go to surgery. It helps put everyone at ease.
After speaking with the patient and their family members, I focus my attention on the anesthesiologist and the anesthesia resident. I tell them my plan and what I need from them. I also answer any of their questions and then they roll the patient back to the operating room.

Remember, the anesthesiologist has already been in the operating room setting-up their supplies. There is also a whole separate team of nurses and perfusionists in the operating room setting-up that the patient hasn’t met yet.
The circulating nurse has temporarily left the process of setting-up the operating room and met the patient and the family. The circulating nurse becomes the conduit to update the family from the operating room during the procedure. The family waits in the waiting area, which is right next to the Pre-Op holding area, during the operation.

After the anesthesiologist has rolled the patient back to the operating room and the patient has kissed their loved one goodbye, I spend 5-10 minutes with my first assist to discuss the technical details of the procedure and what I expect from them. I also tell the first assist what special equipment or instruments I need. The first assistant has reviewed all of the medical records and any x-rays or studies and is familiar with the case before I speak with them. Nevertheless, it is important to have this discussion before we get to the operating room.
Next I take another flight of stairs up to the third floor where my office is. My office is located right above the operating rooms which allows me to get the OR quickly when I need to.
I drop-off my lunch and briefcase in my office and head to an administrative meeting.
There are a lot of administrative meetings that doctors need to attend. There are an endless number of committees and working meetings which help improve the functioning of the hospital and department.
The administrative meeting usually lasts an hour, from 7am to 8am. While I am in the administrative meeting, my patient and operating room team are getting the patient ready for surgery. For aortic surgery cases, this takes between an hour and and hour-and-a-half. No surgery is being done during this time. Instead, the patient is being put to sleep, special IVs and catheters are being placed, the patient is being positioned properly on the operating room table and instruments are being set-up. If questions arise about the preparations for the case while I am in the meeting, the operating room calls me on my cell phone.
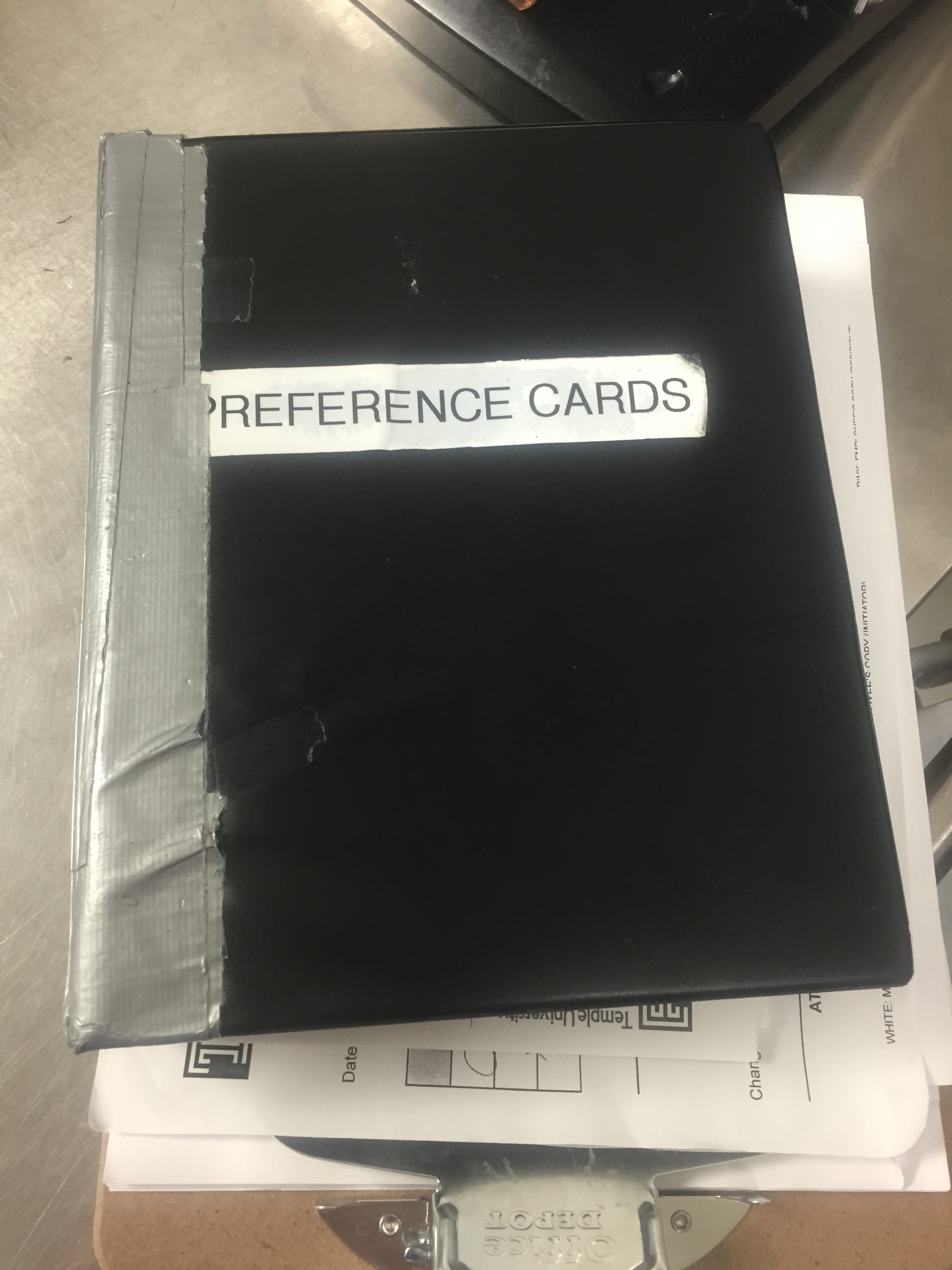
There are a lot of instruments that need to be opened for aortic surgeries. Each physician has a preference card for each procedure they do. This preference card details all the instruments needed and the steps of the procedure. The instruments for the case are resterilized after each case and packaged into instrument trays. That way the scrub nurse doesn’t have open each instrument individually. Sometimes there are over 100 instruments and that would take a long time.
Other disposable equipment is needed for these procedures and is also opened, such as sutures.
Aortic procedures frequently need a surgical or endovascular graft and/or a heart valve. These items are not opened-up until we need them in the middle of the surgical procedure. However, these items come in a range of different sizes. The circulating nurse and the surgical first assistant check to make sure we have all the sizes we need for the operation and put all the boxes in the room to have ready when they are needed in the case. Next to blood availability, the availability of all the special equipment we need is just as critical for a successful case. This will be the first and last things I ask the team. I triple-check to make sure everything is available.
Intensive care unit
After the administrative meeting is over, I head to the intensive care unit and round on any of my patients that are there. I meet with the nurse and our critical care team at the bedside of each of my patients to review their progress. We review their vital signs, lab work, xrays and review a plan for the day.
Because aortic surgery patients are so sick after surgery, they frequently stay in the ICU for several days. In addition, some of these patients need to stay on the ventilator until their lungs and vital signs get stronger.
Office

After rounding in the ICU, which is right next to the operating rooms, I head back up the stairs to my office.
I prefer a clean office, as you can see. I also use a standing desk (more on that later).
By this time, it is 815am. The office staff have arrived and I meet with them to discuss the day. I have a list of items which need to be completed that I give them. They also remind me of my schedule for the day and make sure I am prepared for any meetings that I may have later in the day.
Just like the operating room, it is important to huddle with the office staff to make sure everyone is focused on the day and that we take care of the things we need to.
It is now 830am and I call into the operating room to check on the progress.
Next, I log into my computer, answer a few emails and then review (again!) the patient’s medical record who I am operating on. I focus on every detail I can because you never know what little piece of information may be needed in the care of this patient. I also review all the xrays and CAT scans and once again go over in my mind key points of this patient’s case.
I grab about a half-liter of water from the water cooler and drink it while I am reviewing the CAT scans. Aortic operations can be long cases, and you have to be hydrated to start the case. On the other hand, you can’t take a break during the case, so you don’t want to be too hydrated, if you know what I mean.
By this time the OR is ready for me. They call me when the patient is being prepped with betadine. The patient is under anesthesia, all the instruments are set-up and all the equipment is ready.
The operation
I then head down to the second floor, hang my lab coat on the coat rack and put on a disposable surgical hat and mask. In the hallway leading to the OR, I usually run into a few colleagues and we usually chat or briefly discuss an issue that needs my attention.
I walk into the operating room and usually everyone is busy doing something. I check with the anesthesiologist to get an update on how the patient is doing, I check with the perfusionists to make sure the heart-lung machine is ready and discuss different equipment I need. I then check with the scrub nurse to make sure everything is ready and then with the surgical assistant to ask if there are any new questions.
Finally, we have a “time out”. This is a new policy which has been implemented in all hospitals across the country to ensure patient safety.
The surgical time out is a last check to make sure everything is ready for the procedure. Everyone stops what they are doing, the circulating nurse opens the chart to the signed surgical consent and the anesthesiologist looks at the patient’s wristband with their identifying information. We check to see if the medical record number, name and birthdate match the chart and signed consent. (This is probably the 4th or 5th time it is checked that day).
We then check to see if blood is available, and then I go over with everyone the plan for the case. Once all of the surgical checklist is completed, we then drape the patient with surgical drapes and leave exposed the chest and both groins for a standard aortic surgery.
Next, I grab my operating loupes. Surgical loupes are specially-fitted glasses that have a 2.5x magnifying scope built into the lens. This allows surgeons to focus on very detailed areas of the heart and aorta. I also put on a headlight. This headlight sits on my forehead and shines a bright light into the surgical wound where I am looking. There are bright surgical lights in the operating room, but when we open the chest there can be deep pockets behind the heart which need extra illumination and that is where the headlight helps.
After putting my headlight on and my surgical loupes on, I head to the scrub sink. At the scrub sink, I usually talk with our Cardiovascular service line coordinator about any administrative issues that need my attention. It takes about 3-5 minutes to scrub and this is a good time to have a quick meeting with someone.
It is 845am and we are finally ready to start the operation. Countless people and staff members have helped this patient from the time they arrived to the hospital to the time the operation is ready to start. Without their help, we as surgeons wouldn’t be able to do what we need to do. I try to thank everyone who has helped get this patient ready, but there are so many people I usually can’t thank all the people that deserve it.
After scrubbing my fingers, hands and forearms, I walk into the operating room with water dripping off my arms. I push the door open with my back to avoid touching anything.
Next, I dry off my arms and hands with a sterile towel which is handed to me by the scrub nurse. I then put on my sterile gown and sterile gloves and step-up to the right side of the operating table. The entire team has one last surgical timeout and it is time to begin the operation. It has only been 2 hours since I said good morning to Joe the security guard in the parking lot.
Was this post informative?
Subscribe to my newsletter to learn more about the aorta, its diseases, and how to treat them.
Comments
Share your thoughts below — I try to get back to as many comments as possible.