An Ulcer of a Different Sort: Penetrating Aortic Ulcers
Introduction
Ulcers. Everyone has heard of them. You know, the kind of digestive problem which results from too much stomach acid and is relieved with antacids. The kind that causes stomach pain. You most likely have heard of the term “sour stomach”.
Well, guess, what? “Ulcer” is actually a more general medical term describing a discrete, localized erosion of a biologic surface. In the case of a gastric (stomach) ulcer, there is an erosion of the protective lining of the stomach which causes pain due to the deeper tissue of the wall of the stomach being exposed to stomach acid and is associated with eating spicy foods.
Definition of penetrating aortic ulcers
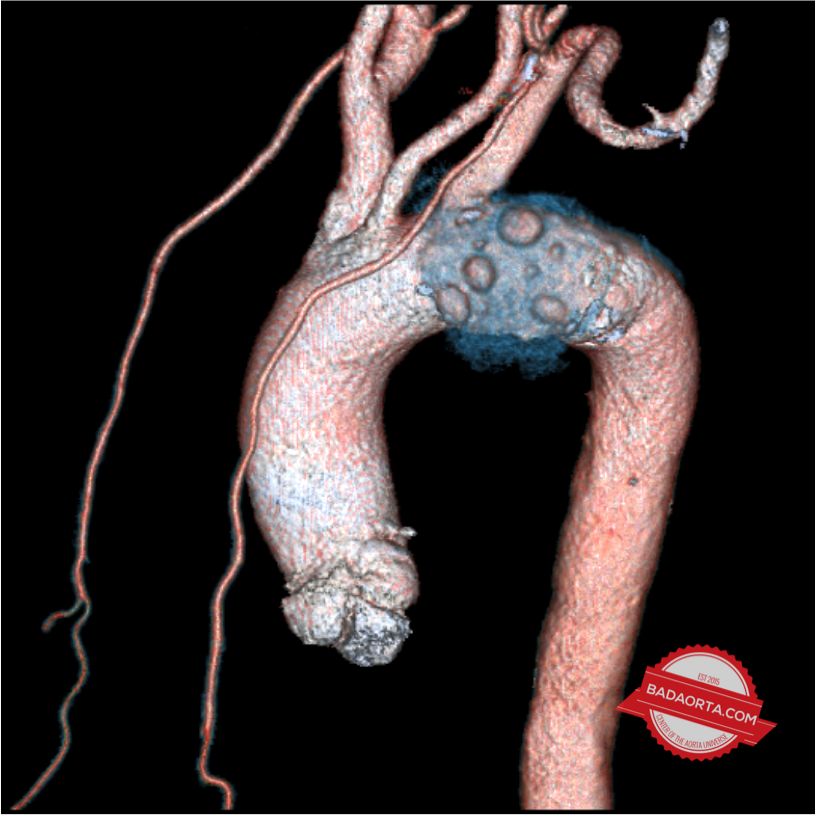
The Aorta, like the stomach, is also prone to developing ulcers. The official medical term is “penetrating aortic ulcers”, or PAU for abbreviation. Another term for this condition is “penetrating atherosclerotic ulcer”. As you recall, the aorta is a blood vessel (largest in the body!). The aortic wall is composed of three layers: intima, media and adventitia.
The intimal layer of the aorta refers to a thin, continuous sheet of cells, called the endothelium, which line the innermost part of the aorta. These cells are in direct contact with blood. Think of your lawn. The sod sitting on top of the dirt is similar to the endothelial layer of the aorta.
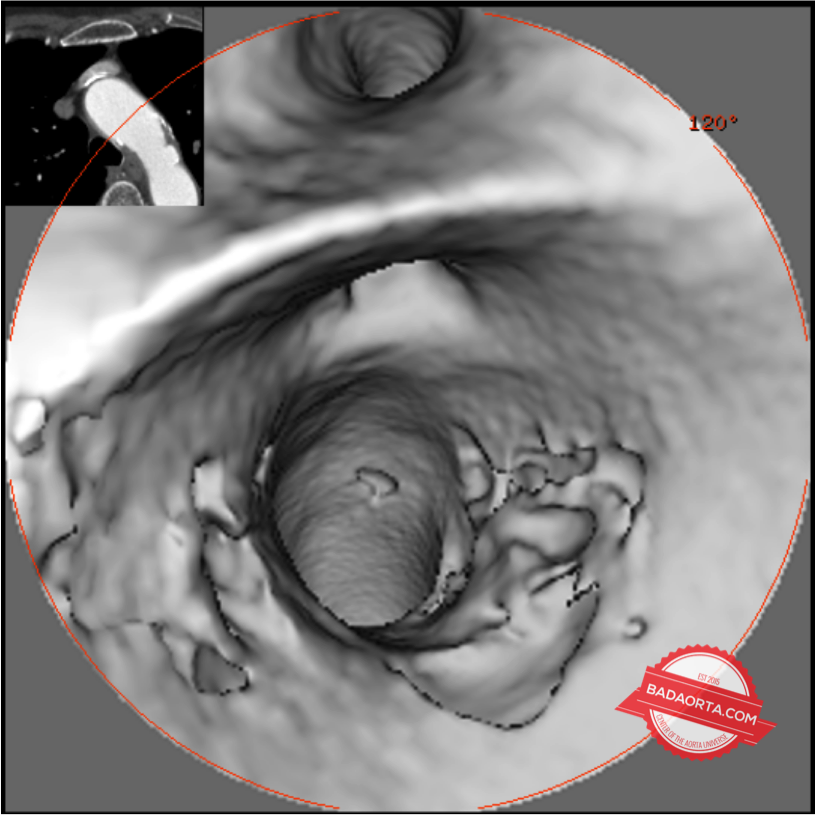
Penetrating aortic ulcers are a medical condition consisting of a focal erosion of the endothelium of the aorta. This means that a small section of the sheet of cells lining the cells of the aorta disappear.
PAUs are part of a spectrum of diseases of the aorta called acute aortic syndrome (topic of future post).
Back to your yard, think of a small patch of dead grass in your lawn where the dirt below is exposed and all grass is gone.
Pathophysiology of penetrating aortic ulcers
In its normal, healthy state, the inner lining of the aorta consists of a glistening sheen of healthy cells. However, the glistening sheen can become dull and irregular as a result of atherosclerotic disease.
Atherosclerosis is a degenerative process, usually associated with aging, where the body deposits both cholesterol and calcium into the lining of a blood vessel (in this case, the aorta).
These atherosclerotic deposits can be either large or small. When there is an excessive amount of calcium in the atherosclerotic deposit (one particular patch of the wall of the aorta), it is called a “plaque”. Plaques can occur anywhere in the vasculature of the body, and when they occur in the aorta, can cause a problem.
The aorta is meant to be a flexible and elastic structure which expands and contracts with the pulse. The pulse represents the dynamic change in the blood vessel associated with blood ejecting from the heart. The heart beat causes a rush of blood out of the heart which forces the aorta to physically expand and contract.
With the stiffening of the aortic wall associated with atherosclerosis as we age, the stresses and strains of the aortic wall change in relation to blood flow. When there is a plaque of cholesterol and calcium, combined with a stiffened aorta, these plaques can suddenly rupture.
When a plaque ruptures, blood seeps below the endothelial cell surface and creates a disruption in the inner lining the the aortic wall.
Viola! This disruption in the aortic wall resulting from a ruptured plaque is a penetrating aortic ulcer. In addition to the ulcer, an intramural hematoma occurs (bleeding into the wall of the aorta).
How often do penetrating aortic ulcers occur?
Penetrating aortic ulcers (PAUs) occur in approximately 7-8% of all patients with aortic disease.
What are the symptoms of a penetrating aortic ulcer?
The most common symptom is back pain. Most patients describe this as a new pain in the mid-back between the shoulder blades. The pain can be either sharp and stabbing or dull and radiating. The sharp, stabbing pain is usually localized to one spot in the back. The dull, radiating pain is usually spread across the entire upper back.
Other symptoms, include chest pain which is similar in characteristics to pain associated with a heart attack. If the penetrating aortic ulcer is located in the abdominal aorta, the pain would be in the low back. 20% of the time, patients with penetrating aortic ulcers have no symptoms at all.
How do you know if you have a penetrating aortic ulcer?
Most of the time you can’t tell if you have a penetrating aortic ulcer. These penetrating aortic ulcers develop suddenly (literally in a heart beat). If the pain is so intense that you have to go to the emergency room, doctors will perform a battery of tests.
If a CAT scan is performed at the time of the emergency room visit (and it should be), then the penetrating aortic ulcer can usually be diagnosed by seeing the erosion and hematoma of the aortic wall.
However, many patients are walking around without any signs or symptoms and don’t have any inkling that they have a penetrating aortic ulcer.
What is the health risk of having a penetrating aortic ulcer?
As mentioned above, penetrating aortic ulcers are part of a spectrum of an acute aortic syndrome. The risk of a penetrating aortic ulcer is that the aorta could rupture. The ulceration in the aortic wall is literally a defect which decreases the integrity of the aortic wall. If aortic rupture occurs, massive internal bleeding could lead to death.
Penetrating aortic ulcers can also lead to aortic dissection. We discussed aortic dissection in a previous post HERE. Aortic dissection is a whole other aortic emergency which also carries a risk of death.
What are the risk factors for developing penetrating aortic disease?
Like most aortic diseases, including aortic aneurysms and aortic dissections, high blood pressure (hypertension), elevated blood cholesterol (hypercholesterolemia) and a history of atherosclerosis increase your risk for developing penetrating aortic ulcers.
For more information concerning the risk factors for developing aortic disease, download your copy of my book here.
What do you do if you suspect you have an penetrating aortic ulcer?
Most of the time, penetrating aortic ulcers are detected through a battery of tests, including a CAT scan, which are performed for new, severe chest or back pain in the emergency room.
If you have any of the risk factors for developing aortic disease mentioned above, then you should be considered to be evaluated by an aortic specialist.
What are the treatments for penetrating aortic ulcers?
Many penetrating aortic ulcers can be managed with medicines. These medicines are intended to significantly control the blood pressure and cholesterol in the blood. If the ulcers expand, they could become an aortic pseudoaneurysm which would potentially need surgery or treatment with an aortic stent.
Likewise, if the penetrating aortic ulcer progresses to an aortic dissection, then the aortic dissection, depending on severity and extent, may need to be treated with aortic surgery or endovascular repair with an aortic stent-graft.
Summary
Penetrating aortic ulcers are an uncommon, but potentially life-threatening, condition arising from a disruption of the inner lining of the aorta. The process is also called penetrating atherosclerotic disease because of the association with the build-up of cholesterol and calcium into the blood vessels of the body (atheroslcerosis).
Question
Before this, did you ever consider that the aorta could be predisposed to developing ulcers just like the stomach?
Share your comments and join the discussion.
Was this post informative?
Subscribe to my newsletter to learn more about the aorta, its diseases, and how to treat them.
Comments
Share your thoughts below — I try to get back to as many comments as possible.