Battle of the Bulge: Understanding Aortic Aneurysms
Introduction
The Battle of the Bulge was a carefully orchestrated, surprise military offensive by the Germans in WWII to recapture the valuable harbor of Antwerp and this offensive caught Allied Forces off-guard. The “bulge” in the Battle of the Bulge refers to the inward bulge of the Allied Forces lines of defense in response to the attack. As we know, bulges can occur in many forms, and when associated with aortic aneurysms, bulges can be deadly.
Anatomy and definitions
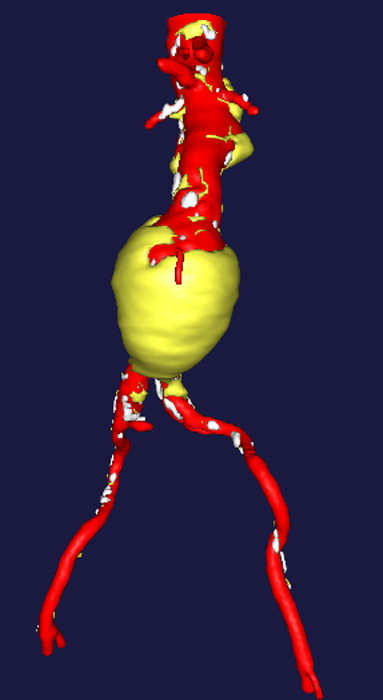 Abdominal aortic aneurysm (AAA)
Abdominal aortic aneurysm (AAA)
Aortic aneurysms are defined as a localized enlargement of a region of the aorta, sometimes referred to as a “bulge” or “bubble”. As you recall, the aorta is divided into several distinct anatomic sections. The diameter, or width, of the normal aorta in each of these regions varies. The aortic segments are: aortic root, ascending aorta, aortic arch, descending thoracic aorta and abdominal aorta.
The overall diameter of the aorta is determined by many factors including: how tall you are, how much you weigh and your family history. For example, the ascending aorta is usually the largest in diameter. There is progressive tapering, however, of the aortic diameter continuously to the aortic bifurcation in the abdomen.
An aortic aneurysm is technically defined as a section of aorta which measures twice the normal width (2 * normal aortic diameter). However, this measurement is relative between patient to patient because of the variability of everyone’s baseline aortic diameter and the variability with the aorta itself.
Nevertheless, any section of the aorta which is greater than an absolute diameter of 3.5cm in width is of concern. This doesn’t necessarily mean that an aorta of 3.5cm always needs immediate treatment, but it is an abnormal segment which potentially can lead to a situation which will potentially need to be treated.
Another term which denotes enlargement of the aorta is ectasia. An ectatic aorta is generally enlarged (non-localized) and may be a marker of an aortopathy (disease of the aortic wall). This is generally a whole different disease process.
Aortic aneurysms
An abdominal aortic aneurysm (AAA) refers to a localized expansion of the aorta in the stomach region. Many people call the region below the ribs and above the waist the “stomach”, but in medical terms it is the abdomen (lower half of the torso). The stomach is technically a digestive organ within the abdomen, not a section of the body. There are many important organs and structures within the abdomen.
A thoracic aortic aneurysm (TAA) refers to a localized expansion of the aorta which develops in the chest cavity (internal to the ribs and breastbone). The diaphragm is a structure used for breathing which divides the chest cavity from the abdominal cavity (roughly in the middle of the torso). The aorta passes through a specially designed hole in the diaphragm which also accommodates the esophagus and aorta together.
There are many risk factors for developing an aortic aneurysm. These include high blood pressure, heart disease, family history and diagnosis of a connective tissue disorder. You may want to check-out our new e-book entitled “Risk Factors for Developing Aortic Disease” to learn more.
When an aneurysm develops, the integrity of the aortic wall (blood vessel) weakens and there is a risk that the aorta could rupture at the point of maximal weakness and result in massive internal bleeding. Aneurysms are a result of a degenerative process.
Symptoms associated with aortic aneurysms
Frequently, an aortic aneurysm does not cause any symptoms. It is usually found incidentally when an X-ray, CAT scan or ultrasound is performed for another medical reason. Most patients are surprised to learn they have an aortic aneurysm. When an aneurysm does develop symptoms, it can be associated with stomach pain, lower back pain, upper back pain or a pain in the chest. The pain is usually described as sharp and stabbing when in the chest and dull when in the abdomen.
Diagnosing an aortic aneurysm
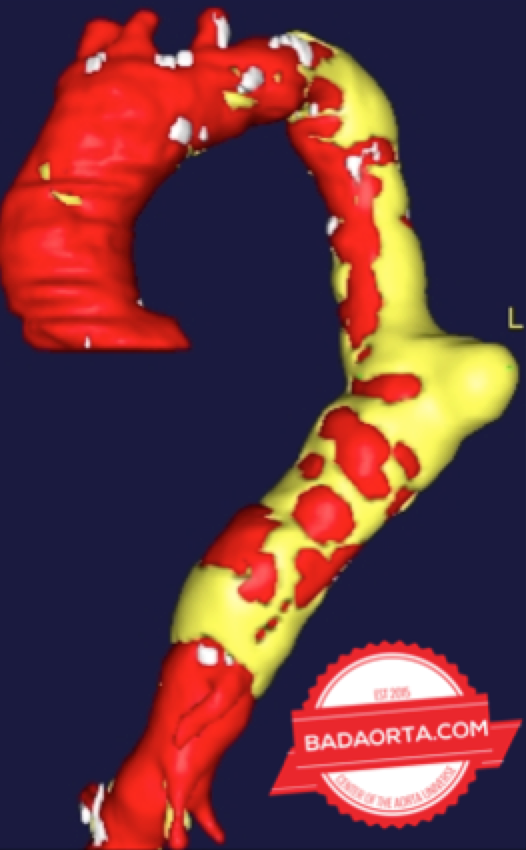
When an aortic aneurysm is detected, whether in the chest or abdomen, additional studies are usually needed. The entire aorta needs to be evaluated from the aortic valve to the aortic bifurcation to make sure that no other section of the aorta is affected with an aneurysm. This usually involves a CAT scan of both the chest and abdomen. This test also allows physicians to also develop potential treatment options.
If the aneurysm is close to the heart (aortic root or ascending aorta), then a echocardiogram (cardiac ultrasound) is needed to inspect the aortic valve. The function of the aortic valve could be distorted by the aortic aneurysm.
Treatments for aortic aneurysms
The decision on when to treat an aortic aneurysm is an individualized one based on patient-specific factors and size of the aneurysm itself. Some aneurysms which are small can be monitored. Others that are larger may need surgery. Options include open surgical repair or endovascular aortic stents. At minimum, patients with aortic aneurysms need their blood pressure well-controlled, oftentimes with medications, to decrease the stress and strain on the aortic wall associated with blood pressure. The higher the blood pressure, the higher the stress and strain is on the aortic wall, which translates into higher risk of aneurysm expansion and potential rupture.
We will discuss the various treatments options for aortic aneurysms in more detail in a future post.
Summary
Aortic aneurysms are localized enlargements of the aorta (bulge) which can occur within the chest or abdomen. These aneurysms are caused by many factors, but results in a weakening of the aortic wall. This degenerative process can lead to rupture of the aorta which would result in massive internal bleeding and death.
Question
Do you know anyone who has been diagnosed or treated with an aortic aneurysm?
Share your comments so that others can learn more.
Was this post informative?
Subscribe to my newsletter to learn more about the aorta, its diseases, and how to treat them.
Comments
Share your thoughts below — I try to get back to as many comments as possible.