The Unfortunate Case of Alan Thicke
[Editor’s note: Download the related podcast to this post on The Dr. Grayson Wheatley Show. Available on iTunes and Android.]
This past week we have all struggled to make sense of the sudden and unexpected passing of the famous and beloved Hollywood actor, songwriter, game and talk show host Alan Thicke.
This has been even more difficult because of his death occurring around the holidays.
With respect to Mr. Thicke’s privacy and the grieving process of his family, I wanted to share what we know about his death and use his unfortunate passing as an opportunity to educate everyone on the life-threatening aspects of aortic aneurysms and aortic dissections so that, from this tragedy, we may help save the lives of others through education and information.
My goal is for the information contained in this blog post to become the pre-eminent source of information available about aortic dissection for the public, medical students, residents in training, internists, emergency physicians and personnel and surgeons.
You may recall a similar situation surrounding the death of another famous Hollywood actor, John Ritter, several years ago from an aortic dissection. As a result of his death, his family set up The John Ritter Foundation, which is dedicated to education and awareness surrounding aortic dissections and other aortic related issues.
Remember: “Every Aortic Dissection is like a Snowflake: Each one is Different.”
Here is what we know so far about Mr. Thicke’s death:
Alan Willis Thicke was born in Kirkland Lake, Ontario, Canada on March 1, 1947.
On the morning of December 13, 2016, the 69-year-old actor was playing hockey with his 19-year-old son, Carter at the Pickwick Ice in Burbank, California. At approximately 11:15am PST, he collapsed suddenly on the ice complaining of chest pains. He was rushed to Providence Saint Joseph Medical Center in Burbank, which is located on the banks of the Los Angeles River and right next to Warner Bros Studios.
According to google maps, Pickwick Ice is 1.1 miles from Providence Saint Joseph Medical Center.
Google Maps estimates the drive time to be 3 minutes in limited traffic between the two facilities, (by standard vehicle, not emergency services ambulance) which is essentially a straight shot down West Riverside Drive.
He expired three hours later at 2:14pm PST in surgery at the hospital.
He is survived by his wife, Tanya Callau, and sons Brennan, Robin and Carter.
Here are news links for more information about Alan Thicke and his death:
According to The County of Los Angeles Department of Public Health Certificate of Death, Mr. Thicke expired from a “ruptured aorta” 3 hours after experiencing a “Stanford Type A Aortic Dissection”.
What Does This All Mean?
Let’s break it down.
I am sharing with you my expert thoughts based on limited information about Mr. Thicke’s case, but in light of an extensive career of treating hundreds of patients with aortic dissections. I can connect the dots in Mr. Thicke’s case from patterns that have emerged from taking care of similar patients with aortic dissections.
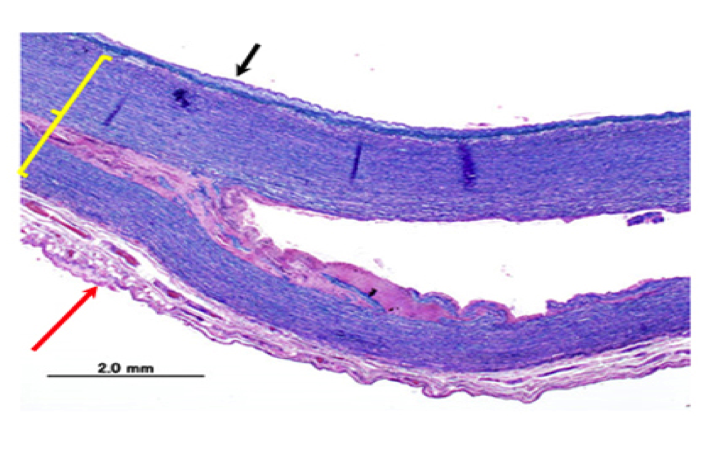
When Mr. Thicke collapsed on the ice complaining of chest pains, he developed a sudden tear, or rip, in his aorta. When this happens to patients, it is sudden and develops within a few heart beats. Prior to the start of the chest pains, the aorta is intact and not torn.
An aortic dissection is a completely different process than a heart attack.
A heart attack occurs from a sudden blockage in an artery (coronary artery) on the surface of the heart providing blood flow to the heart muscle. The chest pain from a heart attack is much different than that of an aortic dissection. Although the aorta is connected to the heart at the level of the aortic valve, an aortic dissection is not a heart attack and not even technically considered a heart problem - although an aortic dissection can lead to a heart attack (more on that below).
The pain associated with an aortic dissection is extreme. My patients describe it as so intense and sudden that it drops them to their knees. They literally fall to the ground and feel an intense tearing or ripping in their mid-upper back and/or their chest.
The aorta is innervated and enveloped with sympathetic nerve endings (think a fine mesh of delicate nerve endings in the wall of the aorta). When there is “trauma” to the aorta (and a sudden tear or rip certainly classifies as a traumatic event), the extensive mesh network of nerve endings send pain signals to the brain.
What is interesting, is that even though the aorta is located in the middle of the chest, the part of the brain that receives the pain signals from the aorta can’t make sense of where the pain signals are coming from. As a result, patients experience referred pain to the mid-upper back (between the shoulder blades or scapulae) which is the best way the body can localize the pain.
It is just the way our brains and body are wired. Our minds and bodies can’t truly differentiate between pain starting in the aorta versus true musculoskeletal back pain. Furthermore, our minds don’t have the innate built-in wiring to discriminate the symptoms between a tear starting in the ascending aorta versus the descending aorta. (Editor’s note:If you need a refresher on the anatomy, check out Dr. Wheatley’s Aortic Atlas.)

However, the rule of thumb for physicians and nurses, is that if the pain is sudden in onset and intense in the upper back: think aortic dissection.
In talking with hundreds of patients with all types of aortic dissections, the common themes are:
-
Intense, sudden onset (out of the blue)
-
The most intense and worst pain of their life
-
Drops them to their knees or they fall over instantly
-
Feels as if they have been shot in the back
-
The pain is most intense in the upper mid-back (between the shoulder blades)
-
Can sometimes feel like a chest pressure instead of a sharp, stabbing pain
-
They can describe the ripping or tearing sensation as the aorta rips
Essentially, prior to the start of the back/chest pain, the aorta is strucurally intact, and is typically not something that has been developing or brewing for a period of time.
When Mr. Thicke went out on the ice to play hockey with his son for the last time, his aorta was intact. We don’t know what types of banging around with other hockey players he experienced while playing, or if he fell down during his session, but in general aortic dissections (tear) do not occur from physical trauma. His activity at the time he developed the chest pains, most likely, had nothing to do with his aortic dissection and rupture.
In rare circumstances, the aorta can tear from major trauma. Called “traumatic aortic transection”, a section of the aorta located high in the chest can tear from a sudden deceleration injury that occurs from a fall from a significant height or in a car accident. [Ed note: future blog post]
In Mr. Thicke’s case, independent of the level of exertion or physical activity associated with his hockey game that day, the aortic dissection was not a direct consequence of the hockey game.
Once the aortic dissection started (i.e. the aorta tore) it became a race against time. With every heartbeat, there was a chance that the tear could worsen or the structural integrity of the aortic wall could give way. Time is always critical in aortic dissections!
Why do aortic dissections occur?
Aortic dissections occur in 2.0-3.5 persons per each 100,000 per year. The average age of onset is 63-years of age. Here is a good publication from Circulation, if you want to learn more.
Aortic dissections are different than aortic aneurysms. Aortic aneurysms refer to a localized enlargement of a portion of the aorta. An aortic dissection refers to a tear, or rip, in the wall of the aorta. An aortic dissection can occur without an aortic aneurysm, and an aortic aneurysm can occur without an aortic dissection. Having an aortic aneurysm increases the chance of an aortic dissection occurring due to a localized weakness and thinning-out of the aortic wall. Understanding the differences between an aortic aneurysm and an aortic dissection are very important and once of the most common mistakes people make.
We don’t know if Mr. Thicke had an aortic aneurysm which predisposed him to an aortic dissection, and it is impossible to tell from the limited information we have been provided.
Even if Mr. Thicke had an aortic aneurysm, he might not have known himself. Aortic aneurysms arise slowly over time and are usually painless and have no symptoms. Even with regular check-ups, he could have developed an aortic aneurysm and not even known about it. He just as likely could have had a completely normal sized aorta.
Risk factors for developing an aortic dissection are uncontrolled high blood pressure, high cholesterol (hyperlipidemia), smoking history, diabetes, family history of aortic disease and a connective tissue disorder, such as Marfan Syndrome or Loeys-Dietz Syndrome.
We don’t know if anyone in Mr. Thicke’s family had a history of aortic disease and we don’t know if Mr. Thicke had highh blood pressure, but I would guess that he has a history of high blood pressure and was on blood pressure medications and possibly statin therapy for high blood cholesterol. In this circumstance, taking a baby aspirin a day doesn’t protect for an aortic dissection.
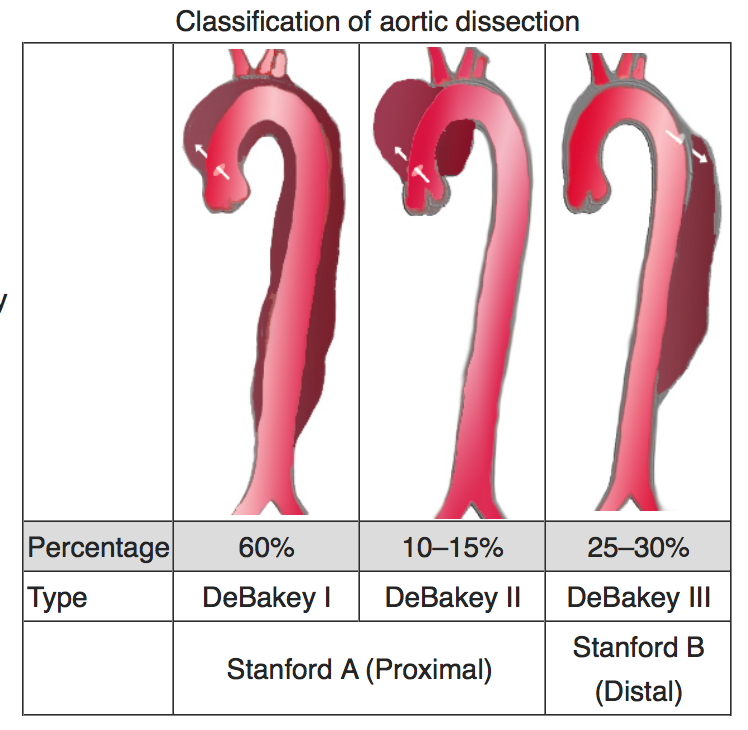
Aortic dissections are typically classified using the Stanford Classification as either Type A or Type B based on the location of where the tear starts. If it starts near the heart, then it is classified as a Type A. If it starts deeper in the chest away from the heart (in the descending thoracic aorta) then is is classified as a Type B. There is also a Debakey classification system. Check out my post “What’s Your Type” to learn more.
Cardiovascular surgeons at the hospital to which Mr. Thicke was transported
According to the Providence Saint Joseph Heart & Vascular Institute, there are 5 Cardiovascular Surgeons and 6 Vascular Surgeons on staff at their hospital.
Immediate heart surgery is required for treatment of a Stanford Type A aortic dissection. Timing is critical to get any patient diagnosed with an acute Stanford Type A aortic dissection to the operating room.
Vascular surgeons do not treat Stanford Type A aortic dissections, because treatment for Stanford Type A aortic dissections involves placing patients on cardiopulmoary bypass (heart-lung machine) and only cardiovascular surgeons are qualified and credentialed to do this.
The five heart surgeons listed to be on staff at Providence Saint Joseph Hospital are (in alphabetical order) are:
It appears that Drs. Capouya, Gheissari and Gottner are all partners in Advanced Cardiothoracic Surgery Medical Group, Inc.

Their group’s surgical outcomes in the Society of Thoracic Surgeons Database are excellent: all 2 and 3 stars which is significantly above average.
Dr. Schaerf is in practice by himself and appears to focus more on Thoracic Surgery (lung surgery) then open heart surgery.
Dr. Yokoyama is also in practice by himself in Pacific Cardiothoracic Surgery Group.
Every emergency room in the United States which has an open heart surgery program has an on-call schedule for patients requiring emergency heart surgery. The call schedule refers to the physician-of-the-day who is assigned to take care of emergencies and consults that come in through the emergency room or transfer center that day. Each day of the week (all seven days) has a heart surgeon assigned to it for a 24 hour period. The call schedule is made up weeks to months in advance, although there can be last minute changes and swaps between surgeons.
Without knowing the call schedule for Providence Saint Joseph Medical Center on Tuesday December 13, 2016, I suspect it was either Drs. Capouya, Gheissari or Gottner who operated on Mr. Thicke.
Putting all The Pieces Together
When Mr. Thicke collapsed on the ice at Pickwick Ice, a 911 call was presumably activated. We don’t know if he was alert, passed out or comatose after collapsing. He certainly was able to communicate to bystanders that he was having chest pains.
We don’t know if CPR was started after he collapsed or if he was even breathing on his own. I am guessing he was in severe pain, but still breathing on his own and talking. Every public facility has an automated electronic defibrillator available which can shock someone who collapses due to an irregular heart beat, and it doesn’t sound like this was necessary in this case.
Once a 911 call is activated, a team of paramedics are dispatched in an ambulance, and seeing how close the ice skating rink was to the hospital, the ambulance was probably there within 5 minutes from the time of the call.
Once the paramedics arrived, Mr. Thicke would have been assessed, started on oxygen and had his vital signs taken. If awake, he would have been asked a few simple questions about what he was feeling and what had been going on. Bystanders would also be questioned briefly about what happened and any other information like if he had been feeling ill earlier in the day or if he had made any other comments about his health. Presumably, his son Carter would have been questioned about any recent or past health problems, including what medications Mr. Thicke might have been taking, leading up to the incident.
Once he was assessed and stabilized, Mr. Thicke would have been placed on a gurney or stretcher, taken quickly to the ambulance by the team of paramedics and transported quickly, with sirens blazing, the 1.1 miles to Providence Saint Joseph Medical Center.
Since the medical center was so close, there would have been no need for an air ambulance to fly him the 1.1 miles to the closest hospital. It is also fortunate that the closest hospital to him had an open heart surgery program. Not all hospitals are prepared or equipped to treat patients with aortic dissections, and only those with an open heart surgery team of doctors and nurses can manage these complex, life-threatening problems.
The paramedics would have radioed ahead during the transportation to the emergency room at the hospital and spoken to the charge nurse of the emergency room and on call emergency room physician. The patient’s vital signs, history and In addition, an EKG might have been taken in the ambulance and transmitted electronically to the emergency room for the ER physician to review to assess for a heart attack.
The ER physician is someone who works only in the emergency room and is specially trained to assess patients with urgent problems and initiate treatments to stabilize patients.
Since this was not a heart attack, the EKG wouldn’t have necessarily been abnormal except for probably a fast heartbeat (tachycardia) due to pain and anxiety.
When Mr. Thicke arrived to the emergency room, he would have been met by a team of techs, nurses and physicians who had been activated. - maybe 5-15 people. He most likely was taken to a special room called the “trauma bay”, even though he wasn’t a trauma patient. The trauma bay is the best place to assess, stabilize and treat emergently unstable patients like Mr. Thicke.
While he was being unloaded from the ambulance and transported by stretcher to the trauma bay, the paramedics would be updating everyone about the current status of Mr. Thicke’s vital signs and any treatments they would have administered. Sometimes family members can accompany their loved one in the ambulance to be close and provide important patient contact information to the receiving team at the hospital.
Not much could have been done in the 2-3 or so minutes it would have taken to travel the 1.1 miles from the ice rink to the hospital. Mr. Thicke probably arrived without an IV in place due to the rapidity in which the events unfolded, and probably just had time to receive oxygen, have his vital signs taken and attached to a heart monitor.
Once he arrived in the trauma bay, a complex, but highly organized process began unfolding. In the triage process, everyone in the room has a role and the emergency room physician is in charge.
Multiple teams of people do their jobs when a critically ill patient arrives, and since emergency room teams are well-trained and experienced, everyone can accomplish their task in the midst of the chaos of the situation.
Nurses and techs would have removed most of Mr. Thicke’s hockey gear in order to assess him and allow placement of necessary IVs and monitoring equipment. Electrodes on adhesive disks would have been placed on his chest allowing nurses to connect him to the heart monitor in the room. A blood pressure would have been placed on his arm, all while the ER physician was asking Mr. Thicke questions and he was assessing his physical condition.
At a minimum, several IVs would have been placed, a blood pressure cuff would have been placed on his arm, he would have been placed on oxygen and he would be connected to a continuous heart monitor. Intravenous fluids would have been started.
Depending on how unstable Mr. Thicke was, he might have needed to be intubated (breathing tube down his throat) to support his airway.
Most likely, his blood pressure was severely elevated. This always happens in the face an acute aortic dissection. The blood pressure can get as high as 240/150 mmHg.
I suspect given the fact that the Mr. Thicke made it to surgery, that he arrived awake and talking but in severe pain. He was probably started on intravenous medications to lower his blood pressure, and after an EKG was taken that did not demonstrate any evidence of a heart attack, he was taken quickly to get a CAT scan of his chest.
Meanwhile, unit clerks would be checking Mr. Thicke into the hospital and obtaining basic information such as name, date of birth, address, phone numbers and family member contacts. If Carter traveled in the ambulance with Mr. Thicke, he would have given this information to the unit clerk to enter in the hospital computer system.
Once he was assessed and stabilized, he would have received some intravenous pain medications to assist with giving him some relief and help decrease his blood pressure. A number of vials of blood would have been drawn and sent to the laboratory for analysis. A portable chest x ray would have been obtained.
Another scenario that could have happened, and that sometimes occurs with massive aortic dissections, is that the blood pressure is low and the heart stops in the trauma bay or during transport. When this happens CPR is initiated to maintain vital signs. The heart can stop in cases of aortic dissection from one of two causes. One, the aortic dissection could have led to an immediate tear and internal bleeding, so that the decreased blood pressure could be a result of loss of blood volume and lack of blood for the heart to circulate. The other reason could be that the bleeding from a Stanford Type A aortic dissection can occur around the heart and in the pericardial sac. This leads to a buildup of pressure around the heart and the heart stops because no blood can be returned to the heart because of the pressure (called pericardial tamponade).
There are several key milestones that need to happen for someone to survive a Stanford Type A Aortic Dissection:
-
They have to survive the initial event
-
They have to get to the closest hospital to get diagnosed and stabilized with blood pressure mediations
-
They need to be transferred to a hospital with an open heart surgery program that is experienced in treating patients with aortic dissections
-
They need to be able to survive long-enough for the OR team to get notified, set-up and coordinated
-
They need to survive induction of general anesthesia
-
They need to be placed on the heart-bypass machine
If they can make it through each of these milestones (and the time it takes to complete these steps), then, and only then, do patients with Stanford Type A aortic dissections have a real shot at surviving. The surgical repair can most frequently be completed at this point, and then it is a matter of seeing how the patient does once the heart is restarted and the effects of the aortic dissection set in.
In Mr. Thicke’s case, I suspect the heart surgeon on call was notified immediately after the CAT scan was completed. At the same time, an operating room would be identified and an operating room team would begin opening surgical instruments. An anesthesiologist would begin setting-up the anesthetic machine and equipment in the operating room and a perfusionist would begin setting-up a heart-lung machine.
Remember, this was all going on around noon on a Tuesday. The emergency room, operating room team, nurses, techs, orderlies, anesthesiologists, perfusionists and surgeons would have all been in the hospital. There may have been other heart surgeries going on which couldn’t have been stopped to accommodate the surgery. Usually, there are only 2 or 3 rooms in the operating room capable, from an equipment standpoint, of doing open heart surgery which Mr. Thicke needed. We don’t know how many rooms were available in Providence Saint Joseph Hospital, or how many of their existing open heart surgery rooms were running at the time of Mr. Thicke’s arrival and emergency.
Most heart surgeries take 3-4 hours, and at 11:15 when Mr. Thicke arrived, most likely the elective heart surgeries that were going on that day would have been finishing-up and therefore, the emergency occurred at the optimal potential time to best ensure that operating room teams and surgeons were available and ready to go.
Thing would have been a little different if he arrived at 2am when most of the on call team would have been at home and out of the hospital. There could have been extra time added for them to arrive in to the hospital (usually 30 minutes). There are usually enough staff in the hospital at that time to begin the set-up, but everything goes a lot quicker in the middle of the day when staffing is more robust.
If the on-call heart surgeon was scrubbed in surgery and in the middle of the case at the time the emergency was called, he would have most likely notified one of his partners to help assess and prepare for Mr. Thicke’s surgery until he could finish his surgery. He just as likely could have been out of surgery, in clinic or between cases.
It usually takes 20-30 minutes to get a full open heart surgery room ready in an emergency because all the equipment and instruments need to be opened and set-up.
Mr. Thicke would have been receiving continuous monitoring and treatments from the time the CAT scan identified the aortic dissection to the time surgery started. If awake, he would have been told about his diagnosis and need for emergent surgery. If awake enough, he could have signed consent, or if he was incapacitated, his son, Carter, would have signed consent for the emergency surgery.
When the operative teams and equipment and room was ready, he would have said goodbye to his son and any other family members at the hospital and been wheeled off to surgery. This is when the anesthesiologist and heart surgeon assume care from the emergency room physician.
Once in the operating room, he would have been intubated by the anesthesiologist, additional intravenous lines and monitors would have been placed and a foley catheter would have been inserted into his bladder. General anesthesia is initiated through a combination of intravenous medications and inhaled anesthetic agents.
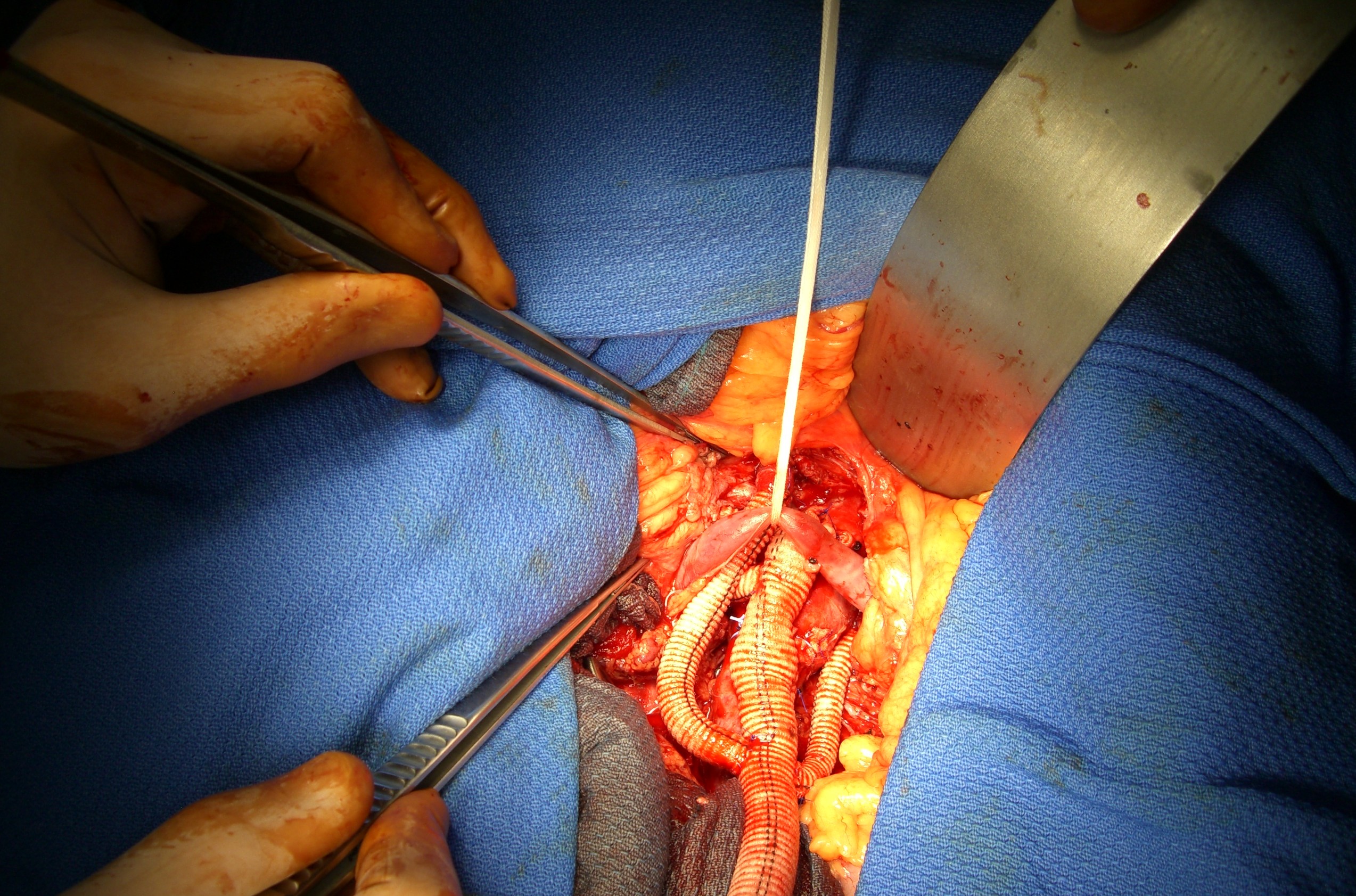
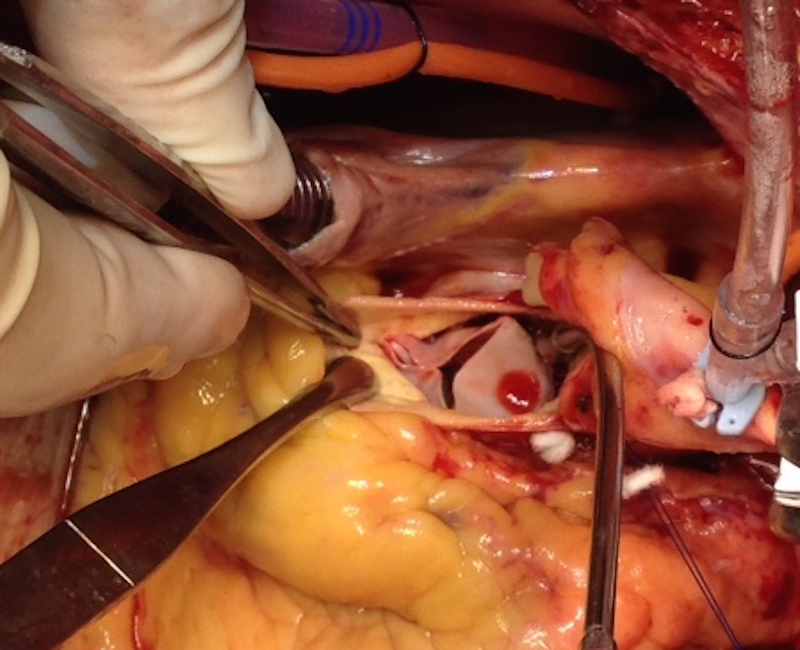
Depending on the operative plan of the cardiovascular surgeon, the most immediate first step would be to place Mr. Thicke on the heart lung machine by surgically exposing the artery and vein in the groin (common femoral artery and vein). Large tube (called cannulas) would be inserted into the artery and vein separately. Once connected to the heart bypass machine, the blood would be circulated in Mr. Thicke’s body by the heart lung machine and his blood pressure would be able to be better maintained with the heart lung machine. It takes about 5 minutes to do this in an emergency situation.
Next, the chest is opened and cannulas (tubes) are inserted into the critical structures of the heart to allow surgeons to stop the heart and protect the heart while it is stopped.
After the heart is stopped, heart surgeons begin by cutting the ascending aorta open and assessing where the aortic tear occurred. The torn aortic tissue is cut out and replaced in the ascending aorta with a synthetic, cloth tube and sewn in place. Sometimes the aortic valve is involved and needs to be surgically replaced as well. Sometimes the tissue is so torn that it becomes impossible to suture it all back together.
We don’t know where in this process that Mr. Thicke passed away, but there are a couple of possibilities.
He could have died in the emergency room before he even got to surgery. This is unlikely, since the reports are that he died in surgery. This would have occurred if the aortic dissection gave way and he had massive internal bleeding before getting to the operating room. No amount of treatments or care can save someone in this situation.
He could have made it to the operating room, but by this time was massively bleeding internally, and no amount of heart lung machine use or surgery could stabilize him in this situation. He would have had to have had essentially no blood pressure and someone would have been giving continuous CPR as he was rolled into the operating room. The survival in these circumstances is less than 1 percent.
Next, he could have had time to have been placed on the heart lung machine, even though he was had unstable vital signs, yet once the operation began the internal bleeding couldn’t be controlled enough or because of the increased pressure inside the pericardial sac around the heart, the heart muscle could have died from lack of blood flow. This is most likely the case for Mr. Thicke.
Finally, the operation could have been completed, but his heart wouldn’t restart after the operation or the tissues were too fragile to be sewn back together. This is unlikely in Mr. Thicke’s case since these operations usually take 4-6 hours to complete, and the death certificate states that he died within 3 hours of the onset of his dissection which is not enough time to complete the surgery.
Summary
As you can appreciate, surviving an aortic dissection is very unpredictable. Many patients with aortic dissection die on the spot and never make it to the hospital. Tine is critical in transporting, diagnosing and treating patients with aortic dissections.
My hope is that the time you have taken to read this information will convince you to share your knowledge with friends and family. 10% of patients with aortic aneurysms are family related and an inherited trait. Furthermore, patients with connective tissue disorders such as Marfans Syndrome and Loeys-Dietz Syndrome are predisposed to high rate of developing an aortic dissection.
Certain patients with known risk factors such as high blood pressure, family history of an aortic aneurysm or known connective tissue disorder need to be screened by a cardiovascular specialist for risk factors that can potentially lead to an aortic dissection.
There is a case to be made for increased awareness for aortic diseases and improved aortic screenings.
For more information about aortic dissections and their treatments, check our my related website drgraysonwheatley.com. Also, feel free to share this page with anyone who you think might benefit from this information or pass is along on social media.
Was this post informative?
Subscribe to my newsletter to learn more about the aorta, its diseases, and how to treat them.
Comments
Share your thoughts below — I try to get back to as many comments as possible.