Transcatheter Aortic Valve Replacement (TAVR)
Aortic stenosis is a devastating disease. It takes years for aortic stenosis to develop. Difficult to detect at first, but eventually the heart’s ability to adapt is lost and patients lose all quality of life.
Over time, the heart gradually enlarges while even simple tasks become unbearable due to extremely labored breathing. Finally, patients with aortic stenosis are unable to move around due to profound shortness of breath.
Fortunately, new minimally invasive treatments have been developed to help patients with aortic stenosis and literally restore their ability to breath and function again.
We are discussing Transcatheter Aortic Valve Replacement, or TAVR, which is a new, minimally invasive therapy for patients with advanced aortic valve stenosis.
Understanding aortic valve stenosis
There are four heart valves. 2 valves on the right side of the heart and 2 valves on the left side of the heart.
Each of the four heart valves have unique functions and properties.
The aortic valve is “last” in the series of 4 heart valves with respect to the flow of blood through the heart. With each heartbeat, blood is pumped (ejected) out of the heart into the aorta.
The aortic valve helps regulate blood leaving the heart and simultaneously prevents blood from returning back to the heart.
The aortic valve normally consists of three distinct leaflets which come together. The leaflets open and close in unison.
The aortic valve can become diseased in many ways, but with regards to the function of the aortic valve, the valve can either be stenotic (narrowed) or regurgitant (leaky).
What this means, is either the opening of the valve leaflets becomes restricted (stenotic) which impairs blood from exiting the heart or the leaflets become incompetent (regurgitant) which allows blood to reflux back into the heart after it has already exited.
Effects of aortic stenosis
Aortic stenosis is a very severe heart problem and can lead to a significantly shortened lifespan if left untreated.
Usually narrowing of the aortic valve occurs slowly over a number of years.

The heart muscle (left ventricle) frequently adapts in cases of aortic stenosis by becoming hypertrophied (thickened) as a result of increased resistance to blood exiting the heart created by the narrowed leaflets of the aortic valve.
Incidentally, the thickening of the heart muscle is a risk factor for sudden cardiac death and can be reversed to some degree with treatment of aortic stenosis.
As you can see in the graph to the right, the survival of patients with aortic stenosis is less than 2 years once symptoms start. As you can see in the insert, the 3 types of symptoms are angina (chest pain), syncope (dizziness or passing out) and congestive heart failure.
When to treat aortic valve stenosis
The decision on when to intervene and treat aortic stenosis is determined by a number of factors. Initially, when the narrowing of the aortic valve leaflets occurs, medications can help relieve the stress on the heart and help the heart adapt.
However, as the aortic stenosis worsens, there comes a point when the heart is unable to compensate for the restriction of blood flow. This stage is classified as “symptomatic”.
There are objective testing and measurements of blood flow and heart function that can be obtained through tests such as cardiac ultrasound and cardiac catheterization.
The gradient across the aortic valve is an important measure of the severity of the aortic stenosis. Gradient across the valve refers to the increased velocity of blood which occurs as blood flow passes through the narrowed orifice of the diseased aortic valve. [bernoulli’s principle]
The criteria on when to intervene on the aortic valve are:
Treatments for aortic stenosis
Once the decision has been made to treat aortic stenosis, there are 2 options: open surgical repair and transcatheter aortic valve replacement.
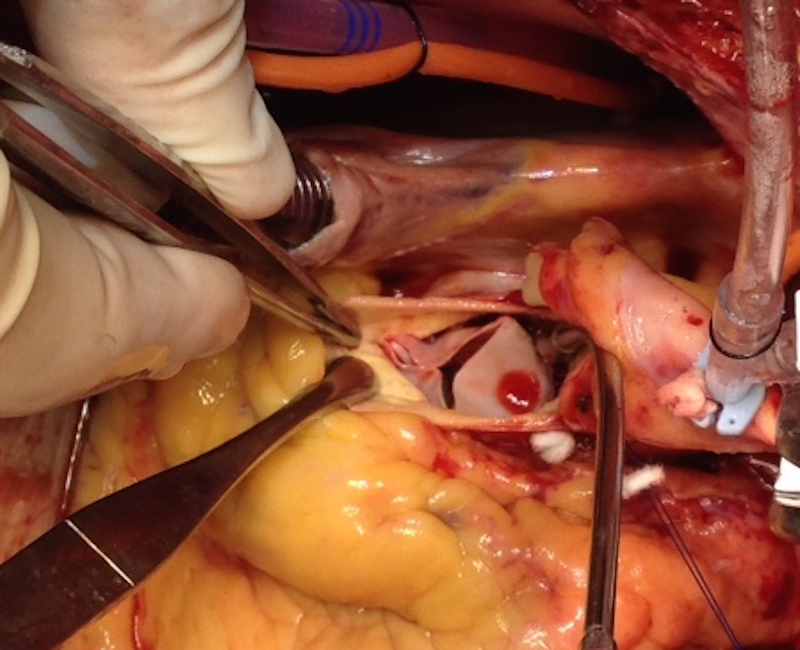
Surgical repair involves opening the breastbone, temporarily stopping the heart, cutting out the diseased valve and sewing in a replacement valve.
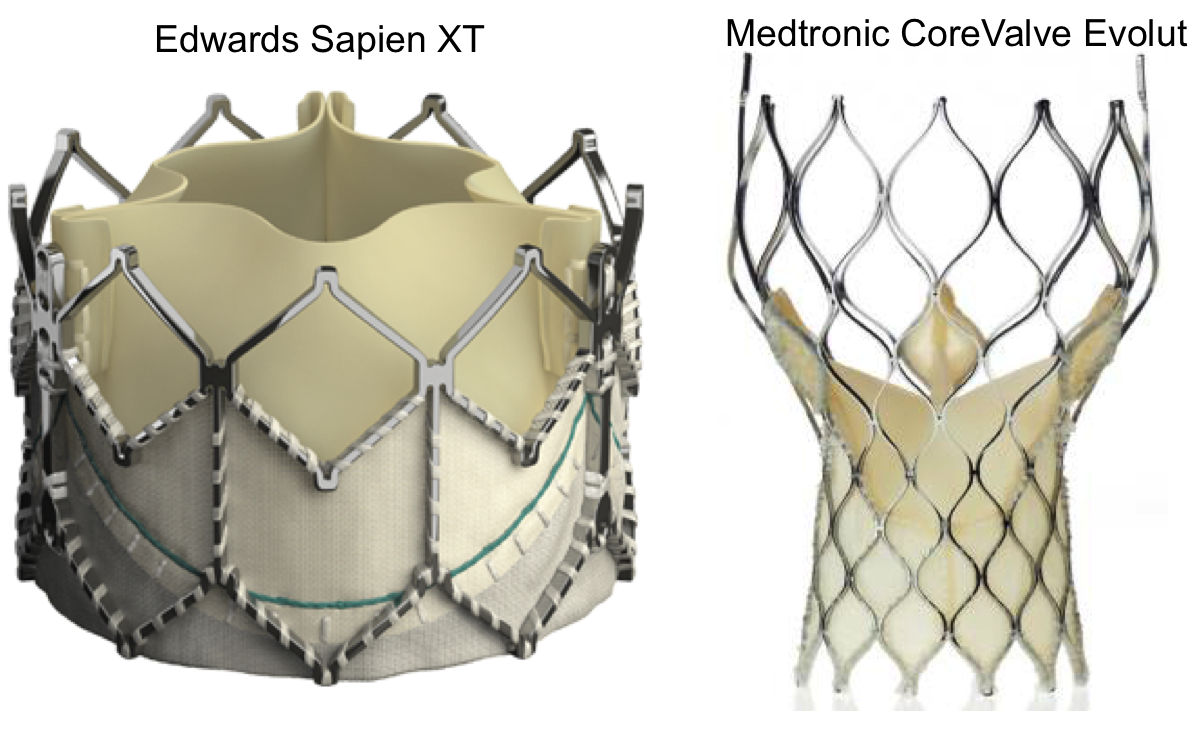
TAVR consists of inserting a catheter (small tube) into an artery (usually in the groin region) and with X-ray guidance, directing the catheter into the heart and releasing the new heart valve inside the old valve. The diseased aortic valve is not removed and is simply pushed aside behind the new heart valve device.
The outcomes of the TAVR procedure are excellent and in high-risk patients are superior to open surgical repair.
Decision making process
There is a complex decision making process in choosing which procedure is best for each individualized patient. Each patient with aortic stenosis is different and unique characteristics such as associated medical problems, overall health and fitness and prior history of heart surgery are just some of the variables that influence the decision making.
In the end, this is an individualized process between the patient and their physician and involves a great deal of discussion.
In summary, aortic stenosis is a challenging disease, with poor survival once symptoms start. There are new treatment options available for patients, but the choice between surgical aortic valve replacement and TAVR is an individualized.
Comments
Share your comments about aortic stenosis and TAVR.
PS. Don’t forget to check out the newly updated Aortic Atlas.
Was this post informative?
Subscribe to my newsletter to learn more about the aorta, its diseases, and how to treat them.
Comments
Share your thoughts below — I try to get back to as many comments as possible.