What's a Little "Kink" Amongst Friends? (Part 2)
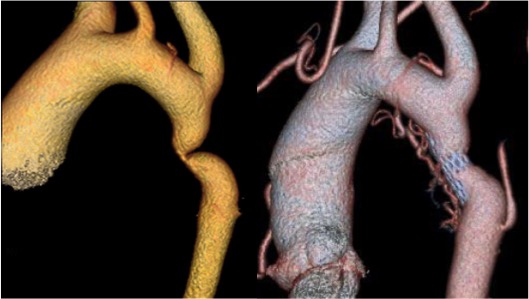
We discussed aortic coarctation in our previous post, found here. As you recall, aortic coarctation is a congenital defect and results in a permanent “kink”, or narrowing of the aorta. This narrowing occurs just beyond the left subclavian artery (blood vessel to the left arm) and is usually found at birth or early infancy. However, sometimes people can grow to adulthood without the defect being detected. The aortic coarctation limits blood flow to the lower half of the body.
Traditionally, aortic coarctation is treated with “open” surgery. Open surgery consists of making an incision on the left chest (thoracotomy). The ribs are then spread and the left lung is pushed to the side. The aorta is then clearly seen and using a set of clamps, the narrowed area (coarctation) is cut-out and the two ends of the aorta are sewn back together.
Sometimes the coarctation is extremely close to the left subclavian artery and part of the artery is incorporated into the surgical reconnection (anastomosis) of the aorta. When this procedure is performed in older children and adults, there is a significant risk for bleeding due to an adaptive increase in the intercostal arteries which run between each of the ribs. These arteries expand significantly in size and can be difficult to manage when opening the chest and spreading the ribs.
With the advent of less invasive techniques, such as endovascular stents, alternative treatments can be offered which are safer and do not involve opening the chest. However, few centers have experience with this type of technique for aortic coarctation. The endovascular skills, techniques and equipment used to treat aortic coarctation are fundamentally different than for aortic-stent grafts used to treat aortic aneurysms and aortic dissections.
We published our experience in the European Journal of Cardiothoracic Surgery in 2010, and I presented our results at a meeting of the European Society of Cardiothoracic Surgery.
The tissue at the site of the narrowing is very rigid and is similar to scar tissue. As a result, it takes a great deal of force to “crack” the ring of scar tissue. Care must be taken not to “crack” the scar tissue with a balloon or stent too aggressively, or else the aorta could tear. The intent of endovascular stents is to improve blood flow through the narrowing to the point that there is minimal disturbance across the treated area (called a gradient).
The endovascular procedure can be performed by inserting the balloon and stent through the artery in the groin (femoral artery) and guided into place using special x-ray imaging. Most of the time no incision is needed at the insertion site (called percutaneous) which allows for a quicker return to full activity and less pain. Most patients stay in the hospital 1-2 nights.
Was this post informative?
Subscribe to my newsletter to learn more about the aorta, its diseases, and how to treat them.
Comments
Share your thoughts below — I try to get back to as many comments as possible.